Week 1 – Part 2: Interning in the Pediatrics Ward
Pediatrics Department
Every Monday at 8am, the staff at the hospital here in Boko gather in the inner courtyard to raise the flag, sing the national anthem, and listen to any announcements from the director of the hospital. It being our first day, we were unexpectedly pulled in front of the crowd to introduce ourselves as the newest interns to the pediatrics and maternity wards. No pressure!
The actual beginning to our day was a bit less ceremonial. We were brought to the pediatrics department where we will spend the first two weeks and were introduced to the nurses who were on shift at the time. We trailed along after them for some time as they did their morning check-in with all the current patients, making sure the files were up to date.
There wasn’t much time for them to give explanations to us as they went, as not soon after a very glamourous woman entered the ward, who we quickly learned was the pediatrics doctor. On her arrival, the staff filed into her office for the morning staff meeting. As we would quickly learn, this was the morning routine in the ward. The head nurses on shift for pediatrics and the neo-natal wards would read through the files of any new arrivals, with the doctor asking questions, and often they would discuss some points, or the doctor would give directions on how certain things should be done.
Sometimes nurses would even be reprimanded during the meeting in front of the group; everyone was expected to just take in on the chin and move on with things without showing any emotion. Most of the time, it turned into a small explanation of how the procedure was meant to be done.
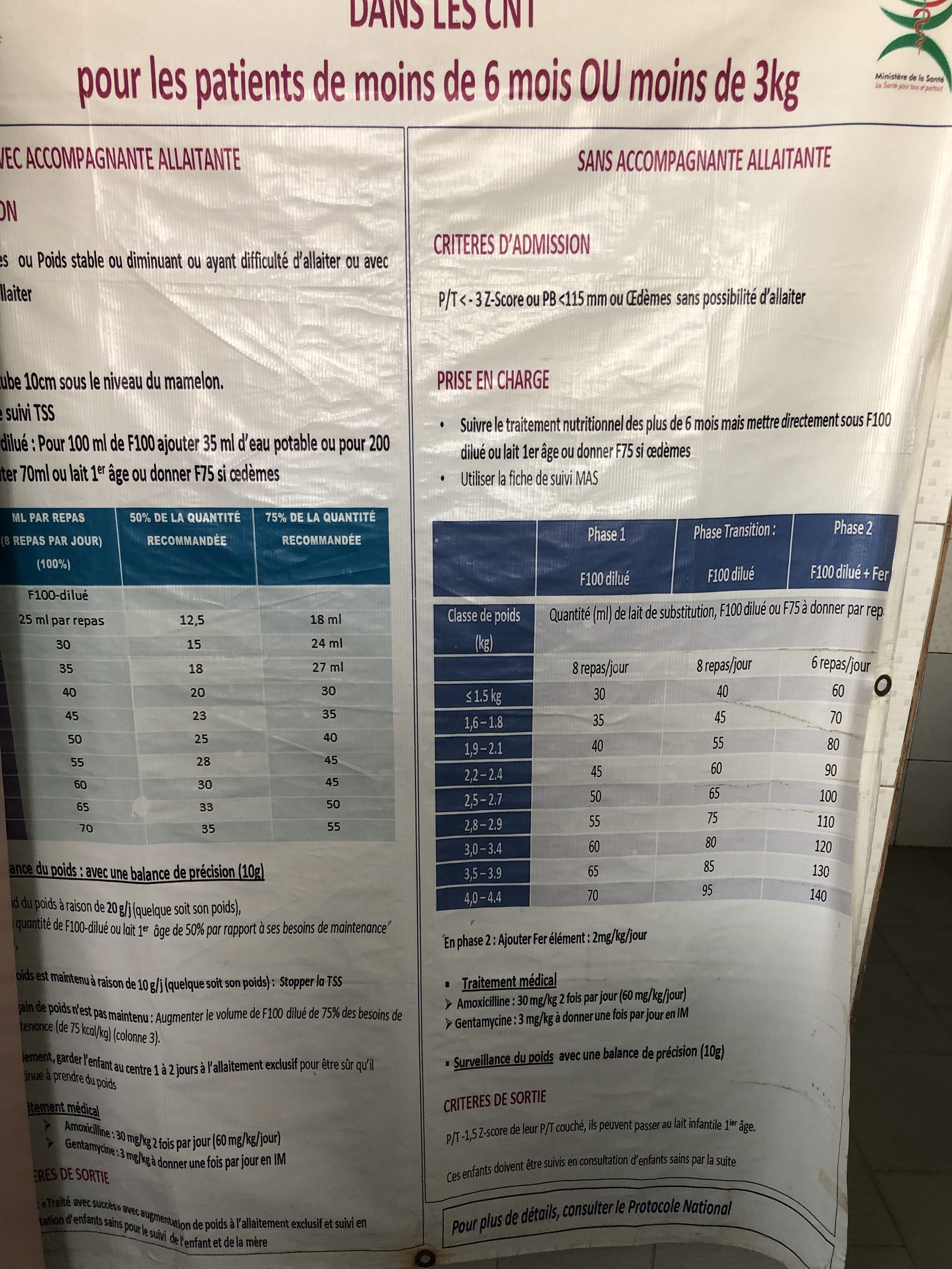
After the staff meeting, the social assistant / nutritionist arrived, whom we are shadowing for our two weeks in pediatrics. It was a bit chaotic for getting started and getting to know how things run in the ward. But we soon learned that in terms of food and nutrition, she is only responsible for the children who are malnourished. In these cases, she is determining how much of what type of food the children will receive and how often, following up daily with their weight evolution and (hopefully) moving them from one phase of nutritional therapy to another.
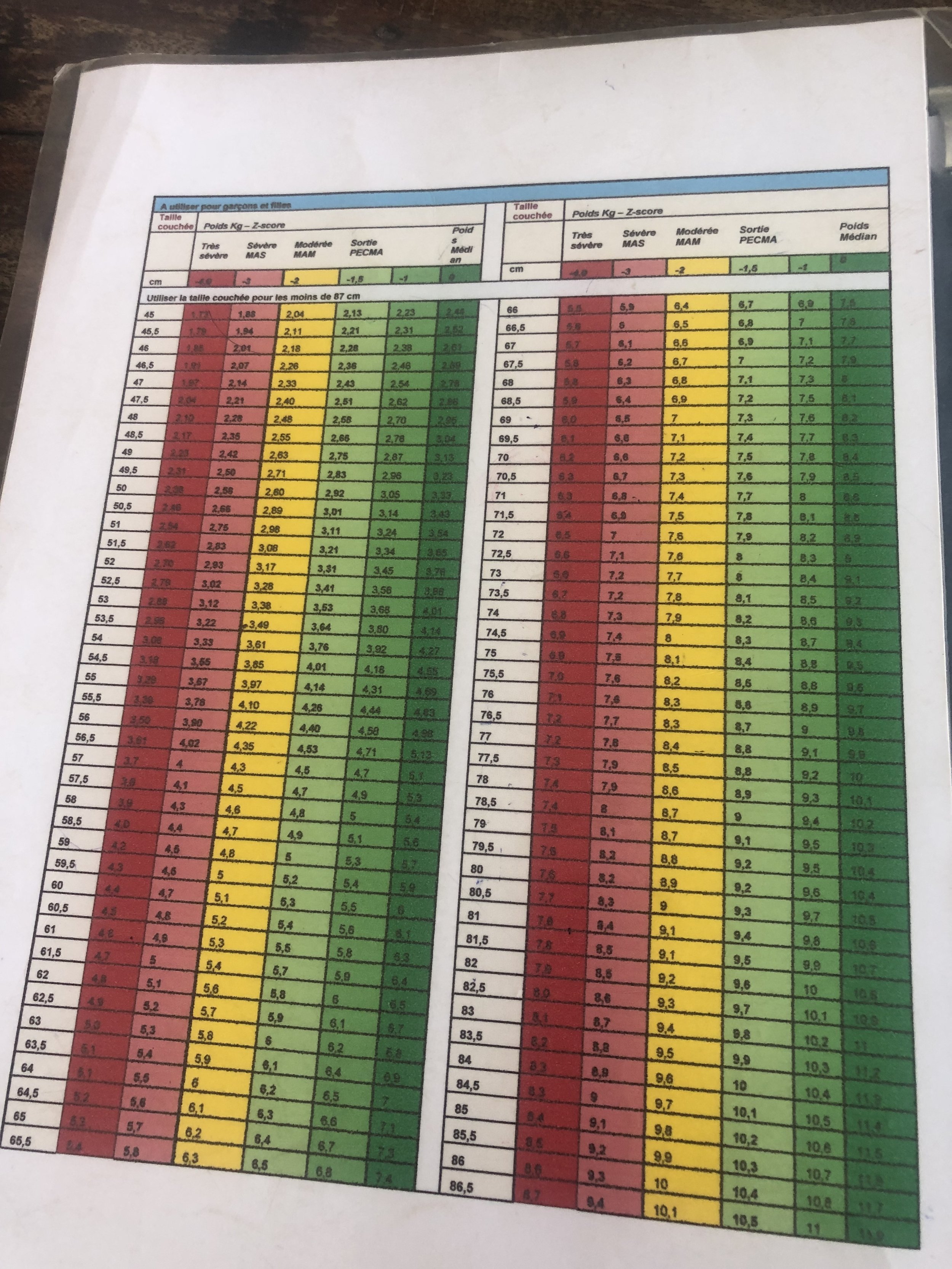
To determine the severity of malnutrition, they use what is called the “z-score” based off the standard deviation of the weight for height. If the child has a score of -3 or more (so 3 or more standard deviations less than the average) then they are considered severely malnourished. If this is combined with “complications”, like oedema, vomiting, or diarrhea then they are referred to the hospital.
The hospital receives from UNICEF powdered therapeutic milk for free – F75 and F100. The children usually start with the F75, which is slightly lower in calories. This is because due to malnourishment, the body isn’t used to digesting food anymore. Starting immediately with too many calories or too high a quantity can result in refeeding syndrome, which generally is a disruption of the electrolyte and fluid balance in the body. In cases of very young children and/or extremely severe malnourishment (younger than 6 months or less than 3kg in weight), they instead use a diluted solution when beginning treatment.
As the child makes progress, such as complications clearing up, ideally within 3-4 days, they are moved from the F75 to the F100 formula. As progress continues, they will then move on to a porridge, called “bouillie” which has been enriched. When they are eventually discharged, the parents are sent home with some packages of the powder to make this broth, as well as packages of “plumpy nut” a high calorie, peanut butter-based product that is also distributed for free via UNICEF.
The children are expected to come back regularly for follow-up check-ins, which take place on Tuesday mornings. Thus, on Tuesday we were busy helping weigh the children, update their files, and give some nutritional advice to the mothers. The mothers could also buy for a small price more of the enriched porridge and also received some free plumpy nut packages. Depending on the Z-score of the child, they were expected either weekly, biweekly, or monthly for follow-up. Unfortunately, we learned that often the mothers don’t return for follow-ups, or they don’t come with the required frequency.
On Thursday we learned that late Wednesday evening a child was admitted with severe malnourishment. However, just after the morning staff meeting it seems things took a turn for the worse. They tried to resuscitate the child, but unfortunately it wasn’t possible. It was a hard situation to witness, although we had come into this experience prepared that we would likely see such a thing occur.
We discussed the story of this child with one of the nurses later in the day and came to find out that the child had be unwell for already a month. However, living quite remotely, with a father who is working away from the home and no means of communication, and a mother who had no transport and other children to look after, the mother just waits until the father returns home. It is only then that the child is brought into the hospital, and in this case, it was just too late. Unfortunately, this seems to be a common occurrence here, and also become worse during the rainy season when remote villages can become practically inaccessible due to flooding.



Health promotion in rural schools
As the larger group of students arrived in Parakou in the run of our first week, we were able to join them for a couple of their activities that aligned well with our internship goals and were also coordinated by our internship mentor, Eric. On Wednesday we joined them to a local school, where the Odisee students had prepared a morning of educational games for the children to teach on topics like proper handwashing, brushing their teeth, and fruit. Femke and I helped with the station on fruit.
The first game was to guess which fruit was in the bag, without looking. Each child in turn closed their eyes and put their hand in the bag to try and identify the fruit. With some of the groups it was pretty easy, and with others less so. The papaya fruit seemed to be especially challenging. The second game they played was the card game, memory. Each child in turn flipped over two cards and the group had to try and find all the matching fruit. It was challenging to coordinate with so many enthusiastic children, but in the end, it was a success. The fruit station finished off by giving each child a skewer with fresh fruit on it – pineapple, banana, and watermelon. We wanted to use the papaya as well, but sadly they weren’t ripe enough yet to eat.
One of the workers at the school also introduced a new fruit to use, that grows on trees locally – the cashew fruit! We’d never seem cashews growing in the wild before. On the end was the nut, that needs first to be roasted and removed from its shell, but it is attached to a red/orange fruit. They don’t tend to eat the fruit itself, but rather bite it open and drink the juice out of it. The juice straight from the fruit had a bit of an apple-like taste to it and left your mouth feeling quite dry.
To finish off our time at the school, we ate lunch together with the children. The group had brought with them big bags of rice and other goods, and the school cooks put together a meal of rice, white beans, greens, and a very spicy pepper and onion-based sauce. We think/hope by the end of our time here we will be well use to spicy food!
Before heading back to our house for the night, we hopped on a zem (the motorcycle taxi) and went to check out a grocery store in Parakou that was started last year by a Belgian couple. It was definitely more in line with what we would expect from a European supermarket (even having some recognizable brands!) but quite expensive, in some cases more expensive than what one would pay in Belgium. We’ve noticed that the grocery stores generally don’t carry fresh fruits and vegetables; for this we will have to go to a local market.
We are lucky, however, that at the entrance to the hospital grounds there are often people setting up stands selling things like fresh fruit and onions, plus there are some stands on the campus itself selling things like bread, yoghurt, coffee, drinks, etc. So we are usually able to pick up the basics without having to venture too far.







Malnutrition screenings in rural villages
On Friday we were back with the big group again for a day of health screenings in more remote villages. There were three groups per village: one doing malnourishment screenings, one for malaria testing, and one for wound treatment. For our malnourishment screenings (which we will also spend several weeks doing later in our internship), we use special measuring tapes to measure the circumference of the upper arm of the child. The armband is marked by colour, showing an indication as to the degree of (mal)nutrition. If the child appears to be malnourished, the doctor from the local health centre will do a full evaluation and either treats the child there, or, if there are additional complications, the child is referred to the hospital. In cases of malnourishment, the Hubi & Vinciane Foundation is covering all the treatment costs.
Our village it was quite chaotic! There were so many people there to see us, and each parent wanted their child to get priority. It was challenging to keep some semblance of order and keep the line moving along at a good pace. After we measured the children for malnourishment and controlled for oedema and anemia, they were sent to get their temperature taken. Any child with a fever immediately had a malaria test taken. Of 10 children with fever, all 10 were positive for malaria – and it is not yet the high season for malaria!
Luckily, we did not find many children with risks for malnutrition. For the children I measured, I had 6 that fell into the “yellow” zone, which meant they received nutritional advice but didn’t yet need to seek treatment. Femke had one child who was in the red zone – likely malnourished – and was sent to consult the doctor from the health centre for further treatment.
Time flew by, and before we realized it, we had been there for almost 3 hours doing tests! And yet the children seemed to just keep coming… It was hard, but at a certain moment we had to announce that it was finished, and we couldn’t continue taking measurements.
It was a long, hot day doing the malnourishment controls, especially considering the time needed to get to and from the village, but it was also one of the most rewarding days thus far.








